Delivering care to patients is only a part, although significant, of the healthcare puzzle. There also backend operations and administrative functions that underpin the entire healthcare system. And one of them is medical billing.
What is medical billing?
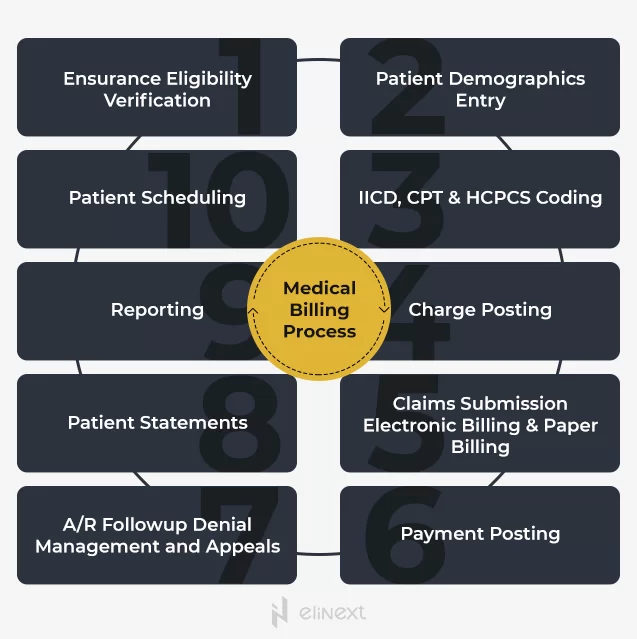
Medical billing refers to the process of collecting patient medical information and submitting medical claims to health insurance payers for the purpose of reimbursement. It is the backbone of the revenue management cycle as without efficient medical billing operations in place, a healthcare facility will struggle to stay profitable and ultimately deliver high-quality care.
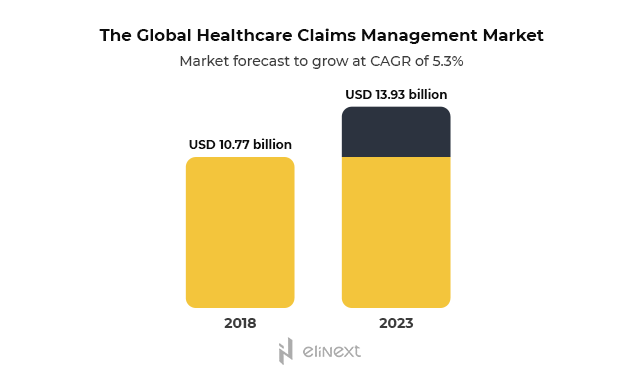
In addition to the immediate gains in the form of reduced paperwork, medical billing solutions accelerate operations, eliminate human errors, and significantly reduce claim rejections. Automated claims management alone can save healthcare providers over USD 11$ billion on an annual basis.
The COVID-19 pandemic has added pressure to the healthcare resources that are already stretched to the limit. Medical billing specialists are now stuck between a rock and a hard place: they need to accommodate an urgent demand and new telehealth services while keeping tabs on continuous changes in medical coding.
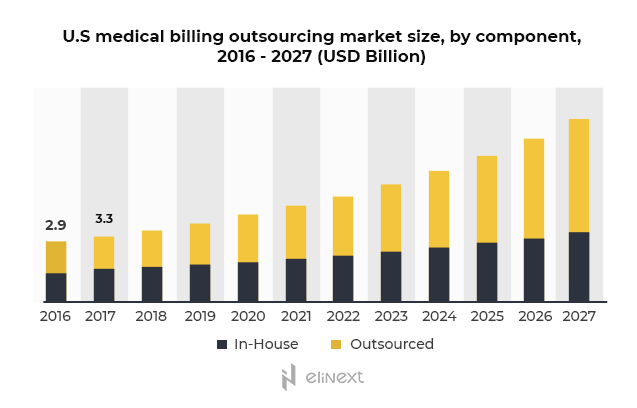
This makes the need for custom medical billing software more pressing than ever, causing healthcare institutions to seek outsourcing vendors to bridge that gap. It is projected that by 2027 the global medical billing outsourcing market will reach USD 23.7 billion.
Whether you choose to buy a ready-made or a custom healthcare solution, here are 7 essential components your healthcare billing software must have.
Key components of a medical billing solution
Eligibility verification
Eligibility verification is often neglected — less than 25% of physician practices have proper checks in place. However, reliable insurance verification can go a long way towards maintaining a healthy revenue life cycle.
Insurance contracts can be complex and confusing, so patients may be not fully aware of all the details affecting their out-of-pocket expenses. Real-time patient eligibility verification includes a range of data like insurance coverage, benefits, co-pays, deductibles, demographics, and more to accelerate check-ins, reduce the risk of rejected claims and also provide patients with all the details so they are not blindsided by hefty bills.
Automated medical coding
To ensure a healthcare practice is reimbursed correctly and in full amount, accurate medical coding is imperative. Medical coding means translating the billable information from medical reports, diagnoses, and medical procedures into unified medical codes. And the International Classification of Disease (ICD) has over 70,000 procedure codes and 69,000 diagnosis codes. To add to the complexity, there were over 500 changes to the codes just last year.
Medical billing solutions can automatically detect errors in codes and flag any inaccuracies or inconsistencies for further review. Augmented with AI capabilities, these solutions can take automation to the next level by combing through clinical documents and extracting relevant information. This computer-assisted coding (CAC) can significantly improve coding accuracy and accelerate the entire workflow.
Electronic claims management
For any medical practice, half of the success lies in effective claims management. Medical claims management encompasses a variety of tasks — patient data entry, claims updating and submitting, tracking and reconciliation. If not automated, these time-consuming responsibilities can easily overwhelm your medical staff, affect overall performance, and hurt the bottom line.
Therefore, a medical billing solution needs to support the following functions:
- Comprehensive claims scrubbing
- Electronic claims submission
- Fraudulent and/or duplicate claims detection
- Claims tracking and status monitoring
- Claims denial management
- Integrated remittance management
Integration with EHR/EMR
Electronic Health Records (EHR) and Electronic Medical Records (EMR) are quickly becoming a vital part of the healthcare industry. By 2017, 96% of non-federal hospitals had HHS-certified EHR systems. So, if you have an EHR/EMR system in place, your medical billing software needs to play nicely with it (or any hospital or practice management system, for that matter).
By bringing these systems under one roof, you will get a comprehensive platform that will serve as a single source of truth, reducing any information gaps and providing a 360-degree view of patients at all times. This, in turn, saves time for all your medical staff and gives a much-need efficiency boost.
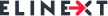
Reporting and billing analytics
At best, the amount of financial data generated by medical billing software can be confusing. This data, however, harbor meaningful insights into your practice performance and financial health, which can be used to support data-driven decision-making.
Choosing a medical billing solution with granular reporting and billing analytics capabilities enables greater visibility into your internal processes, including reimbursement trends, key performance indicators, top carriers analysis, A/R aging. By seeing the bigger picture supported by data, you can pinpoint opportunities for improvement and growth.
Source: Elinext
HIPAA compliance and security
A solid security posture is a must for all healthcare solutions. Since a medical billing system has access to sensitive information like personal and financial data, it must employ robust technical safeguards like data encryption in transit and at rest, multi-factor authentication, role-based access control, and more.
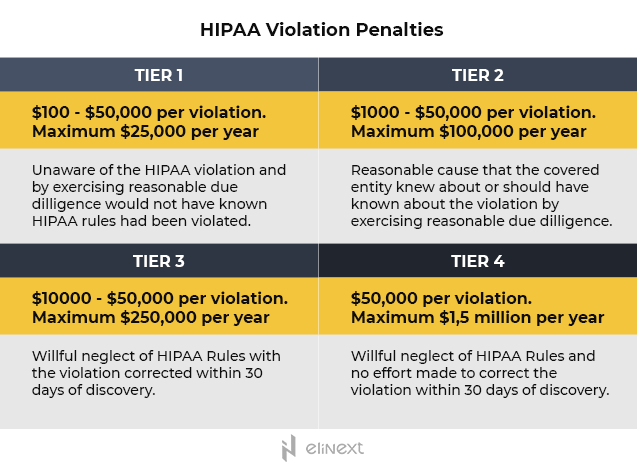
Also, a healthcare billing solution must comply with HIPAA regulations designed to protect the privacy and confidentiality of patient data. Financial penalties for non-compliance can be rather hefty, with fines varying based on the perceived level of negligence, the period of time a violation persisted, the number of affected persons, and other factors.
The bottom line
Medical billing solutions can streamline time-consuming and resource-intensive administrative workflows, reduce human errors, and significantly improve your medical practice efficiency. To reap these benefits, make sure you choose the solution that supports eligibility verification, medical coding, automated claims scrubbing and processing, reporting, and data-driven analytics.
But even with a wide variety of ready-made solutions, your medical practice may have unique needs that require a tailored approach. Look for a software outsourcing vendor who understands the nuances of the healthcare industry like HIPAA compliance and has integration expertise to make the medical billing solution a welcome addition to your healthcare ecosystem.