“Health care is becoming more digitized and consumer oriented. It’s not an overnight change, but more like how summer turns into fall – gradual yet very perceptible.” – Greg Scott, Principal, Deloitte Consulting
In the era of steady technological advancements, data is a synonym for power. How does this relate to healthcare? In a visual representation, PGHD could be depicted as a wrecking ball meant to take healthcare outside the limiting walls of a hospital or clinical facility, thus paving the path for innovation and improving and broadening the patient’s care journey. In today’s article, we will try to dispel doubts by answering 20 PGHD-related frequently asked questions.
-
What is PGHD?
ONC defines PGHD as follows: “Patient-generated health data (PGHD) are health-related data created, recorded, or gathered by or from patients (or family members or other caregivers) to help address a health concern.” Put simply, we are talking about health-related digital information that is recorded, shared, and used outside traditional clinical settings and hospitals.
-
What does PGHD include?
According to the same abovementioned source, “PGHD include, but are not limited to: health history, treatment history, biometric data, symptoms, lifestyle choices.” Notable technological advancements in AI, wireless solutions, or sensor technologies have made it possible for patients to monitor a wide range of parameters: sleep patterns, stress levels, blood sugar levels, surgical wound healing, treatment adequacy and compliance, biometric physiological parameters, etc.
-
Is PGHD a new concept?
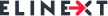
By no means! PGHD is, basically, an advanced, technologized version of the verbal interactions that take place during traditional medical consultations, interactions that offer clinicians valuable insights into the patients’ symptoms, everyday habits, self-evaluation records, etc. Accenture summarizes the PGHD adoption process as follows:
-
What consumer technologies provide PGHD?
When we talk about consumer technologies, we talk about devices that consumers can purchase without a prescription. Wearable blood pressure monitors, diet apps (e.g. Lose It!, MyFitnessPal, etc.), wearable activity trackers (e.g. Fitbit, Apple Watch), or smart insoles (Digitsole Smart Insoles) that not only count the number of steps one takes but also provide biomechanical measures (e.g. impact force, stride length, or propulsion speed), are only some of the available solutions thought out to motivate patients to actively participate in the management of their chronic conditions and overall health.
-
What medical devices provide PGHD?
The RPM technology (i.e. Remote Patient Monitoring) allows clinicians to monitor patients’ health outside the traditional clinical settings by means of remote health monitoring devices (e.g. continuous glucose monitors, Bluetooth scales, blood pressure monitors, etc.), RPM platforms (e.g. Current Health, CareSignal, etc.), clinical dashboards (e.g. eCareCoordinator), wearables (e.g. OnePulse Smartwatch, BioButton), etc.
-
What are the steps that lead to the creation of PGHD?
PGHD creation relies upon various steps:
- Data acquisition
- Data transmission and storage
- Data analysis
- Feedback and decision-making
7. How is data acquired?
PGHD is created from passive and active data sources. When we talk about active sources, we talk about information obtained directly through questionnaires, surveys, etc. mHealth apps, sensors, or smart devices are passive sources of information.
-
How is data transmitted and stored?
There are various ways patients may transmit data to their clinicians: sending a picture by e-mail, physically sharing data with the clinician, manually via portals, etc. However, in the era of digitalization and impressive communication tools, data is usually transmitted automatically to an intermediary server, be it a health monitoring server or the app’s server.
-
How is data analysed?
Without analysis, PGHD would be useless. PGHD can be analysed by the healthcare professional directly, by software installed in the app/device itself, by intermediary people or software, and even by other people in groups created on social media.
-
What are the digital health categories that have received the most funding?
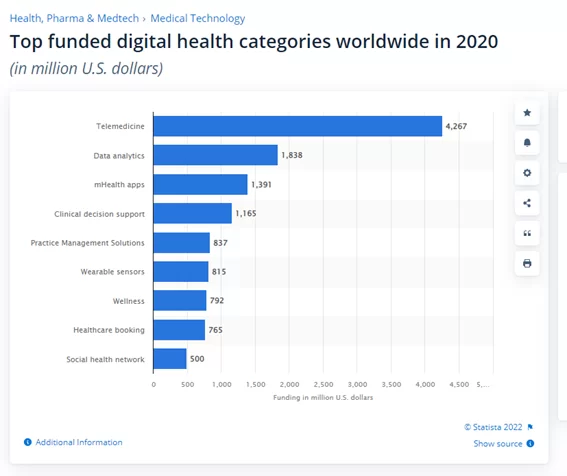
Source: https://www.statista.com/statistics/736163/top-funded-health-it-technologies-worldwide/
According to this statistic, and under the clear influence of the pandemic, funding for telemedicine reached over 4.2 billion U.S. dollars. However, data analytics, mHealth apps, and clinical decision support haven’t been neglected either, validating a tendency: PGHD empowers both patients and healthcare providers.
-
Which mHealth apps are expected to dominate the market by 2025?
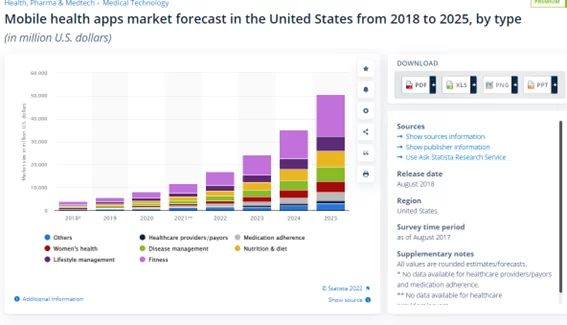
Source: https://www.statista.com/statistics/889582/mhealth-apps-market-size-forecast-by-type-in-the-us/
With fitness apps clearly dominating the chart, by 2025, apps related to lifestyle, nutrition, diet, and disease management are expected to reach 7.5 billion U.S. dollars.
-
Is the global remote patient monitoring devices market size set to grow in the coming years?
According to Fortune Business Insights, in 2020, the market size was USD 30.05 billion, with the cardiovascular disease segment dominating the market.
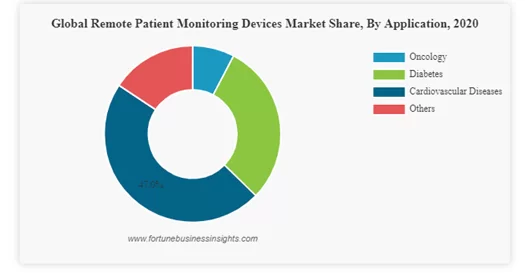
According to the same source, the global remote patient monitoring devices market will continue to grow at a CAGR of 18.9%, reaching USD 101.02 billion in 2028.
-
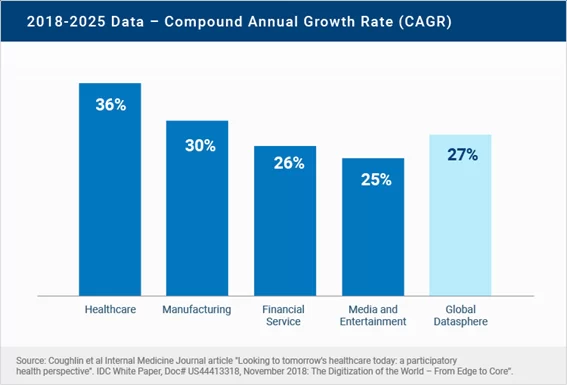
How much data do patients generate?
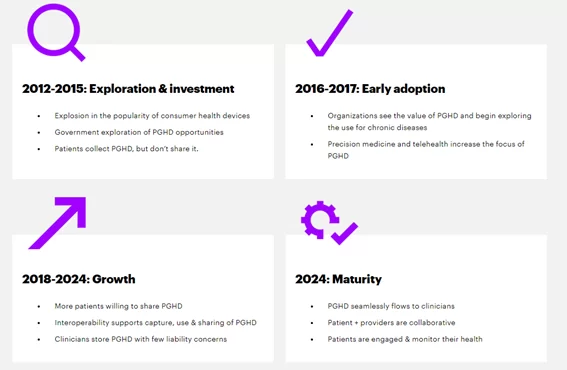
EMRs, EHRs, an extensive range of wearables, sensors, and apps, and the list can continue. As pointed out by RBC Capital Markets, 30% of the data generated globally comes from the healthcare industry. Boosted by the digital revolution, the impressive collection of healthcare data is expected to grow at a CAGR of 36% by 2025, outperforming sectors such as manufacturing, financial services, and even media and entertainment:
-
How does PGHD change the patient-clinician relationship?
Basically, PGHD acts as a gap-filler between physical consultations, fostering the bidirectional, continuous interaction between patients and clinicians and empowering patients to play an active role in their health outcomes. Since patients themselves are responsible for collecting and sharing their own health data, PGHD enhances the feeling of autonomy and engagement.
-
Under the present circumstances, can we talk about PGHD literacy?
Back in 2018, Looking to tomorrow’s healthcare today: a participatory health perspective summarized the ‘health digisphere’ as follows:
Source: https://onlinelibrary.wiley.com/doi/10.1111/imj.13661
For this scheme to continue to be relevant and functional, both patients and clinicians need to keep up with the fast-paced technological advancements.
-
What are the main benefits for patients?
PGHD offers a series of notable advantages:
- Enhanced patient care: clinicians can make quicker and more informed decisions
- Improved patient outcomes: allows clinicians to make well-informed care plans, thus preventing potential complications
- Improved coordination between specialty care teams
- Enhanced patient awareness, engagement, satisfaction, and sense of autonomy
- Improved chronic and preventive care management
-
What are the main benefits for clinicians?
Among the multiple benefits PGHD offers clinicians, we could highlight:
- Provides clinicians with valuable data that would be impossible to obtain otherwise
- Provides a clearer and more accurate vision of the patient’s overall health status
- Provides valuable insights into disease causes and risks
- Reduced costs by lowering readmission rates and reducing errors
- Plays a crucial role in public health surveillance and clinical research
-
What are the main PGHD-related challenges?
- Difficulties to integrate PGHD into clinical workflows due to a series of factors such as lack of proper training in its usage, huge variety of interfaces and data types, deficient data integration and management across systems, etc.
- Concerns about personal health data privacy, security, and secondary use
- Lack of standards for wearables and mHealth apps that may lead to concerns about the accuracy of the registered data
- Limited – and in some cases even non-existent – access to broadband Internet (e.g. rural areas), expensive technology, etc.
- Liability for medical decisions based on PGHD
- The huge amount of data may turn into a burden for clinicians and generate unrealistic expectations from patients’ part
-
What requirements should PGHD meet to support decision making?
According to an article published in NIH in December 2019, Patient-generated health data management and quality challenges in remote patient monitoring, PGHD must be:
- Accurate
- Complete
- Accessible
- Understandable
-
Can PGHD revolutionize healthcare?
The use of innovative technologies such as AI, ML, predictive analytics, or blockchain can provide unprecedented medical insights, paving the path for innovative, value-based, patient-centred, ethical, and secure health services and products.
To sum up…
With the digital health tech industry steadily growing and diversifying, there is no wonder that PGHD is exponentially changing the healthcare ecosystem, empowering patients to become key stakeholders in their own care plans and improving clinician-patient communication. Despite limitations and concerns, PGHD creates real opportunities for value-based, patient-centred care.