“It’s crazy to me that in this world of electronic medical records Walmart has so much information about how we shop, but no one has that information about our health. Why can’t my doctor say, ‘Wow, Anne, based on your lifestyle and behavior, you’re five years from being diabetic. But I can go to Target, and they know exactly what I’m going to buy,” stated Anne Wojcicki, CEO of 23andMe, back in 2015, highlighting the role big data could play in healthcare with the right approach. Over the years, all the stakeholders in the healthcare sphere (Yes, that includes patients!) have been slowly getting comfortable with the idea that information technology will keep the momentum high on improving and digitalizing healthcare. Just try to remember when was the last time you have seen a doctor taking notes on a piece of paper. Difficult to remember, right? The implementation of EMR, EHR, and PHR has streamlined the communication between healthcare stakeholders, paving the path toward safe, accurate, patient-centered, and preventive care.
EMR – What is it exactly?
EMRs (i.e. Electronic Medical Record) are software solutions thought to store crucial patient data such as:
- Medical, surgical, family, and social history
- The doctor’s notes
- Medication
- Allergies
- Treatment plan
- Demographic data
- Test results
- Immunizations
- Billing information
Put simply, EMRs are the digital equivalents of traditional, hand-written (often illegible!) medical paper charts. Unlike medical paper charts, EMRs do much more than store patient data. EMRs can be used for e-prescribing, billing, ordering lab tests, messaging, or granting patients easy access to medical data using online portals (e.g. test results, medication tracking and reminders, appointment reminders, progress notes, vital signs tracking, self-care and educational information, etc.)
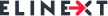
Unlike EHRs, which can be defined as inter-organizational systems that support the exchange of information, EMRs are local, internal organizational systems (e.g. limited to a single clinic, hospital, etc.) We have already mentioned that EMRs are digital versions of paper-based medical charts. Even though EMRs are easily accessible and offer more functionalities than their paper counterparts, they do have a weak spot: they are stored locally and are not interoperable. Simply put: no medical record gets out and no medical record gets in.
EHR – What is it exactly?
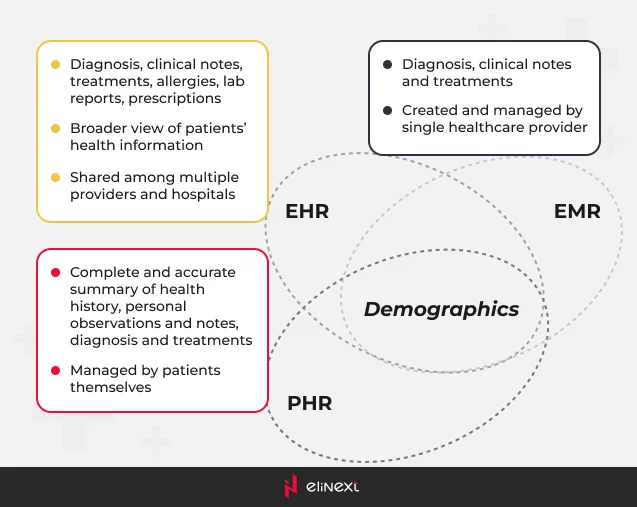
Another type of digital version of paper-based medical charts, HealthIT defines EHRs as “real-time, patient-centered records that make information available instantly and securely to authorized users.”
EHR systems go well beyond storing a patient’s medical history, offering a comprehensive view of the patient’s past, current, and even future health status. Remember the interoperability factor we mentioned above? What distinguishes EHRs from EMRs is the fact that they include data from ALL the authorized parties involved in the patient’s care – starting with specialists and ending with pharmacies or private clinics – and facilitate the exchange of information between them. As a matter of fact, EMRs and PHRs can be considered data sources for EHRs.
EHRs store data such as:
- Personal information
- Medical and surgical history
- Demographic data
- Medication
- Treatment plans
- Immunizations
- Allergies
- Lab tests
- Diagnoses
- Clinical imaging
- Progress notes
- Billing information
In addition, EHR systems can be used to:
- Report outcomes
- Access and analyze real-time data
- Support evidence-based decision-making
- Improve the communication between patients and physicians
- Enhance preventive care
- Prescribe electronically
- Send reminders and warnings
- Provide valuable clinical data for medical research, drug development, etc.
- Automate workflow
- Bill fast and accurately
PHR – What is it exactly?
With similar features to EHRs, PHRs are patient-centered systems that patients manage directly in a confidential and secure environment. Basically, EHRs and PHRs store similar health data: medical history, medication, demographic data, immunization dates, allergies, diagnoses, etc. However, PHRs are enabled to store information that comes from other sources as well:
- Patients can enter relevant data manually (e.g. over-the-counter medications, diet plans, etc.)
- Information derived from home-monitoring devices (e.g. wearables, pulse oximeters, glucometers, blood pressure cuffs, Bluetooth scales, thermometers, etc.)
Put simply, PHRs allow patients to take control of their own well-being, thus enhancing engagement and empowering them to make well-informed decisions about their health.
According to HealthIT, there are two main types of PHRs:
- Standalone: this type of PHR is usually stored on the patient’s computer. The patient can decide whether the recorded data is shared or not with other parties involved in his care plan.
- Tethered: this type of PHR is linked to an EHR and patients use secure portals to access their records.
EMRs Vs. EHRs Vs. PHRs: synopsis
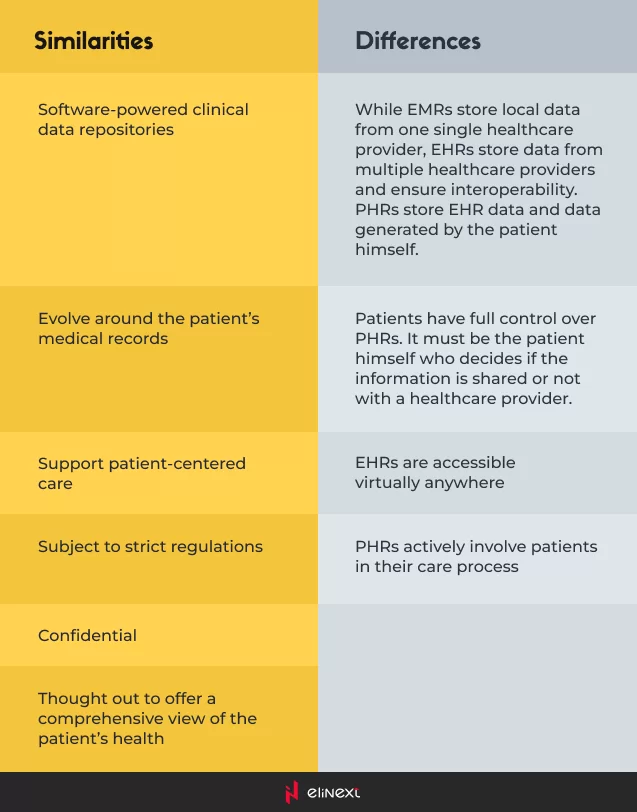
This diagram perfectly summarizes all of the above:
Are EMR, PHR, and EHR systems here to stay?
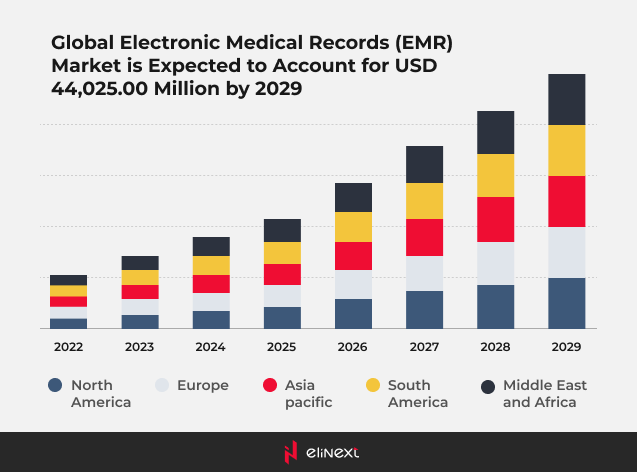
In 2021, as Future Market Insights highlights, fueled by the outbreak of the COVID-19 pandemic, the global EMR market size reached $21.5 Billion. Data Bridge Market Research estimates that, by 2029, the global EMR market will reach $44 Billion.
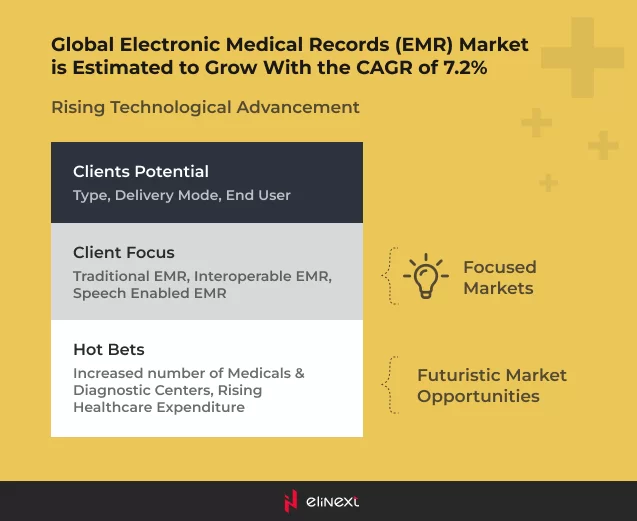
The same source foresees a bright future for PHRs and identifies multiple market opportunities:
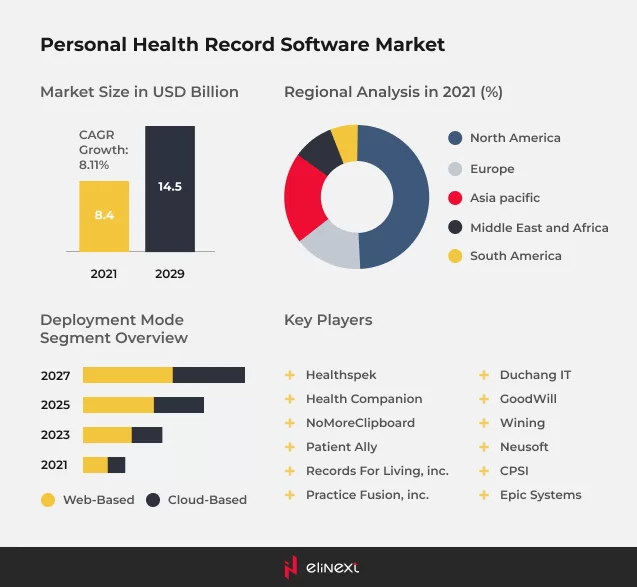
According to MMR, in 2021, the global PHR market was valued at $8.40 Bn. By 2029, it is expected to continue to grow at a CAGR of 8.11%.
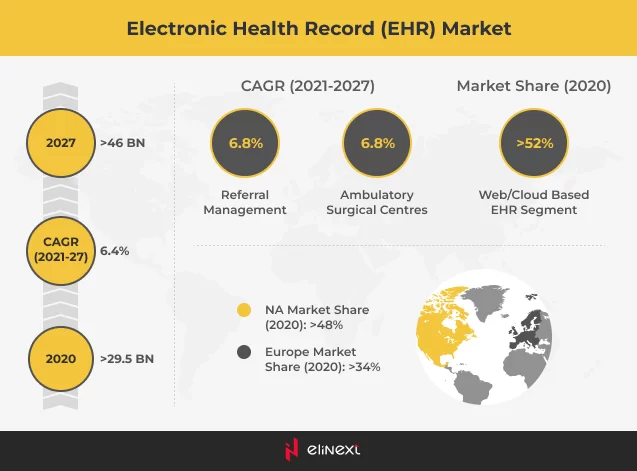
According to Global Market Insights, in 2020, the EHR market was valued at $29.5 million. By 2027, it is expected to keep growing at a CAGR of 6.4%, reaching $46 billion.
It certainly does look like EMRs, EHRs, and PHRs are not going anywhere any time soon.
Wrap up
The presence of digital technologies in all facets of our lives is indisputably solid. Despite implementation hurdles, legislative uncertainties, or security, privacy, and liability concerns, the integration of EMR, EHR, and PHR systems in healthcare paves the path toward the much-coveted patient-centered medical approach. The combination of health records, demographic data, behavioral patterns, and lifestyle choices – all compounded with innovative technologies such as blockchain, AI, NLP, or ML – is a powerful concoction that will substantially improve patient and public health.
Boasting broad experience in Healthcare software development, Elinext provides tailor-made solutions such as the Measure Builder Project.